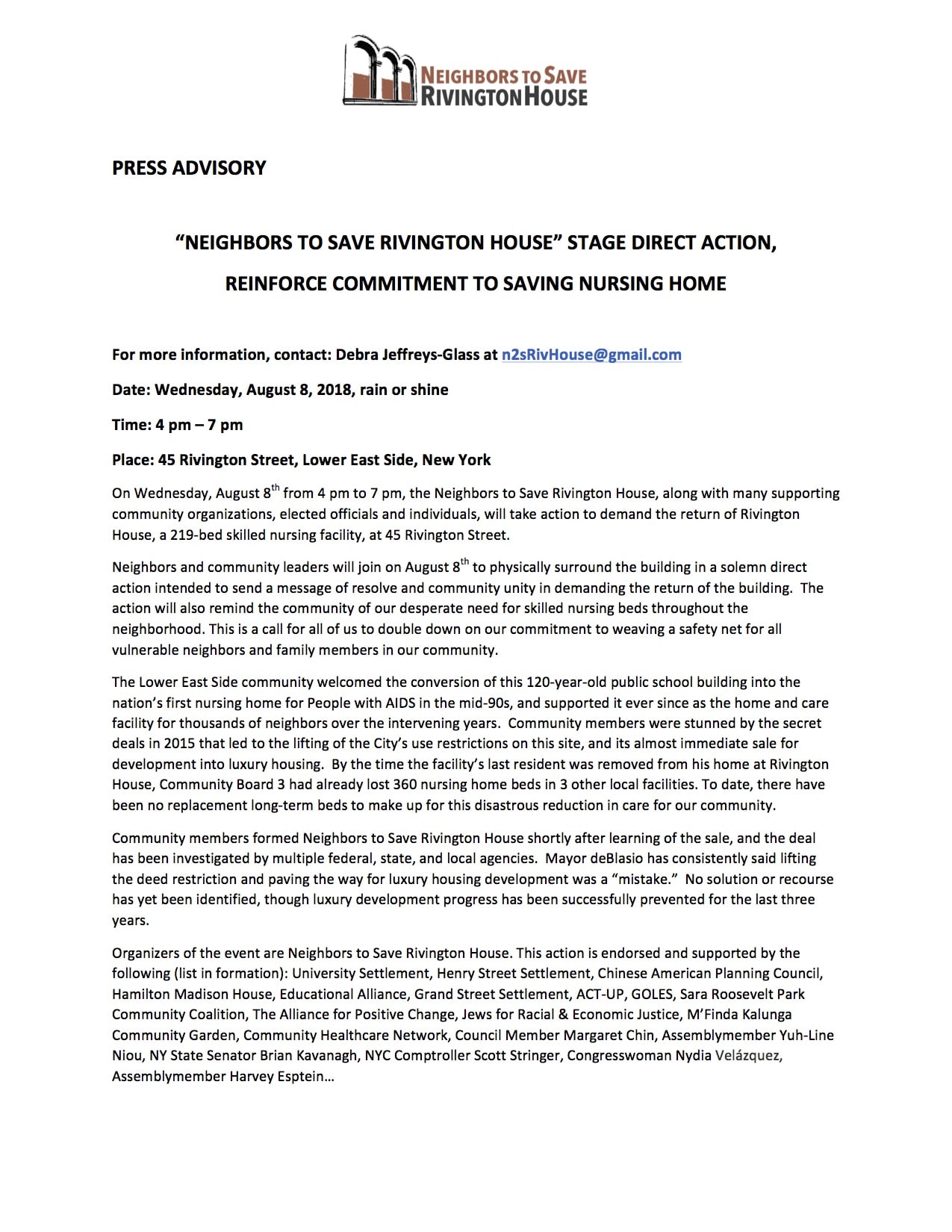
From Neighbors to Save Rivington House Update:
Press coverage (thank you to our local media – never more important). Quotes:
“…in a letter from CM Chin and Man. Borough President Brewer to Dep Mayor Alicia Glen, [both insisted that] Rivington House should not be converted into residential use. [arguing] that while the building itself predates current zoning regulations, its conversion to the type of residential space Slate wants to create violates the area’s 2008 zoning agreement because of … infrastructure burdens. .. the question of whether to approve the conversion is at the discretion of the Department of City Planning, and the council member’s office has been talking with lawyers from the city about ways to get the building back to its previous use. “Considering how the deed restriction was lifted and the transaction was allowed to go through, we’re still exploring every opportunity legally that the city has to take back this property,” – Paul Leonard on behalf of CM Margaret Chin’s Office.
“It’s the neighborhood, the building, but most of all the people I miss the most. I’m still very angry and upset about what happened … Basically, I think Allure should be punished for what they did to us.”…
“I wasn’t supposed to make it past 48,” he said—described the “really great experience” he had while receiving care at Rivington House, recalling his daily walks to the post office, and how students from the Julliard School would come to perform for patients. I just loved the neighborhood. It’s the people…Everybody was on a first-name basis, even the administrators, It was a place to live—Rivington House! We need this place back.” – Richard Rosenberg 70, former resident of Rivington House diagnosed with AIDS in 1994 and told he had two years to live.
“I’m the only one that can go visit her regularly. Once in a while one or two people go visit, but it’s not the same, I want her to live longer and be happier, I don’t want her to go into [depression].” – Sally Roldan forced to place her 84-year-old mother in the Bronx where it takes her more than two hours to visit — one way.
“..I had looked forward to in my retirement that I may see some of the work I’ve done in the park… If I get sick, I would like to be close to my community—the one that I spent so many years developing and nourishing. I would like my final days to be here in this community. Right now, if a senior gets sick, there’s no place for him. There’s no nursing homes. There’s nothing right here for us. And there should be. This has always been a building for the community. And it should always be a building for the community…We’re not going to give up. We will never give up. Never. – Bob Humber Park Warden of Sara D. Roosevelt Park for the past 28 years
“This could’ve been turned into so many really wonderful beds for homeless people or for people with dementia or just really people with chronic illnesses,” Shields said. “I mean, the place was perfectly set up.” – Rosemary Shields former nutritionist at Rivington House
My friends who live down here have been fighting for this building for over three years. And I’ve been hearing about it and inspired by the idea that you don’t have to just gripe about gentrification. You can actually fight it. And so I’m coming here hoping that it’s infectious. And it’ll motivate me to organize people to fight gentrification. –Ela Thier, supporter
I work for the Alliance for Positive Change. ..working mostly with HIV and other chronic illnesses…I’m here, first of all, because it’s my community. This block is special to me because …This is where, [when] I was maybe 12 years old, I used to come to buy $2 bags of dope. Eldridge Street right there used to be the drug capital of the Lower East Side. A lot of big drug dealers came out of here. And they contributed a lot to the spread of HIV… the one good thing that was left of this block was this house. And the mayor sold it. This was the only thing helping people who were adversely affected by drugs on this block. And he just sold it. He sold it like a bag of dope…My cousin who is here right now, she has been HIV positive for a long time. She’s doing great, but she was here one time. She was hospitalized here. If this wouldn’t have been here, she probably would have died.
– William Gonzalez, lifelong LES/East Village resident
“…As family, friends and neighbors maybe all we have is our determination to care. You can’t always stop mistreatment, but you can always oppose it… And sometimes, when we act, we win a few.” – K Webster N2SaveRH
“Neighbors to Save Rivington House has always advocated for the return of the building and that’s still our stance. No matter what the little pieces are, there has not been a replacement for the 219 beds in Rivington House.” – Debra Jeffreys-Glass N2SaveRH
“Something that has fallen off the radar is HIV housing and the need for it, once we had the effectiveness of treatment, people lost track of how dire the need for housing is, and we are trying to get that back.” -Jason Rosenberg, a member of ACT UP New York,
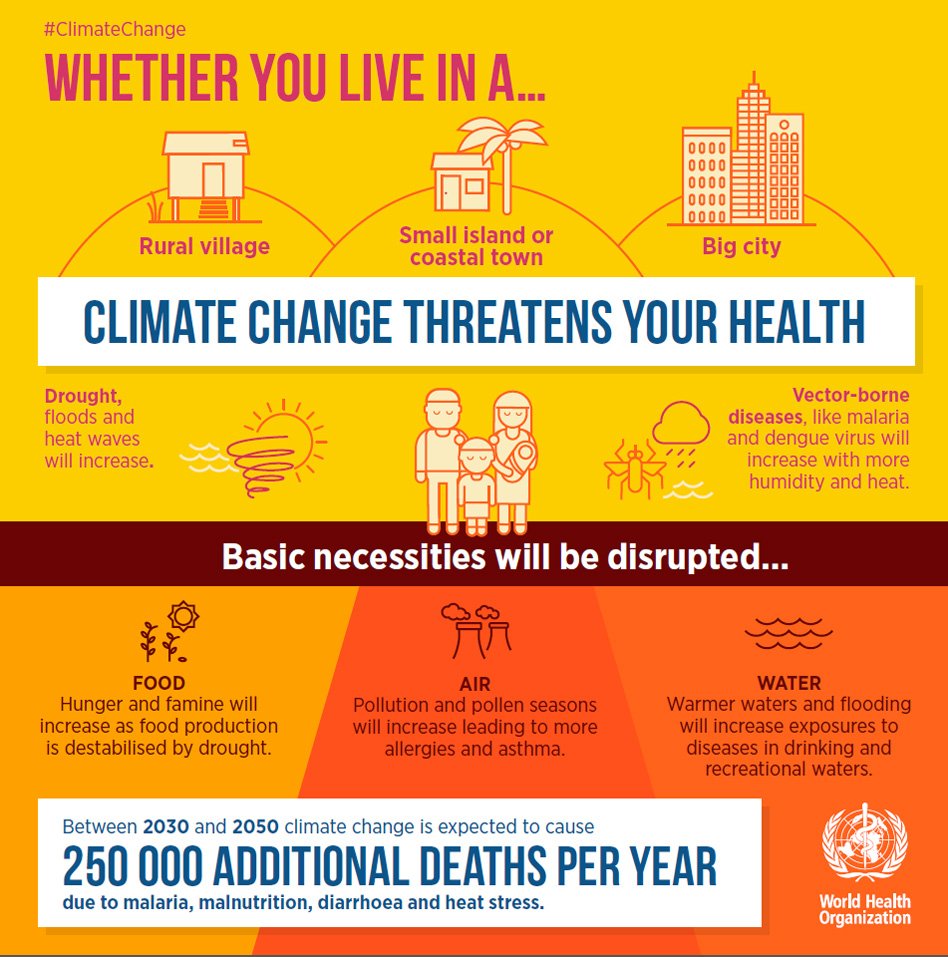
“According to the New York City Department of Health and Mental Hygiene, in 2016, there were 385 new HIV diagnoses of New Yorkers over the age of 50. And, while new diagnoses are declining overall, there was an increase in new diagnoses among women (including transgender women) over the age of 50 from the previous year. Of all those over the age of 50 diagnosed with HIV, nearly 26% also received an AIDS diagnosis.” –George Kevin Jordan, for “The Body”
“The building should’ve been maintained as a nursing facility and there was a terrible bait and switch and terrible dereliction of duty by city officials. “The city should proactively give this facility back and get out from under what was basically a bait and switch in the first place,” Stringer said. “So we continue to come out here and protest, and it also shows that without [an] affordable housing plan that really speaks to issues of healthcare and also true affordability, then the city is going to continue to gentrify and become unaffordable for the very people who moved to the Lower East Side when no one wanted to live here and built this community.” …“You modify a facility — you don’t close it. The list is endless in terms of the needs of a community as it relates to healthcare. There’s a tremendous pressure on the healthcare system in this city. – NYC Comptroller Scott Stringer
“All of us have parents and all of us have bodies that break down every once in a while. So all of us are vulnerable and are going to need healthcare at some point, We know that as people get older and need nursing care, they need to be near their loved ones”…of Slate’s intentions for the property: “This is a part of gentrification.” – Melissa Aase ED University Settlement.
Articles about the Vigil:
Gothamist http://gothamist.com/2018/08/09/rivington_house_les.php
Patch https://patch.com/new-york/lower-east-side-chinatown/compensate-lower-east-side-rivington-house-sale-locals-urge
Bedford & Bowery http://bedfordandbowery.com/2018/08/residents-hold-vigil-for-former-les-nursing-facility-sold-by-the-city-like-a-bag-of-dope/#
CurbedNY https://ny.curbed.com/2018/8/10/17672628/lower-east-side-rivington-house-activists
BoweryBoogie https://www.boweryboogie.com/2018/08/neighbors-demand-return-of-rivington-house-with-vigil/
The Villager http://thevillager.com/2018/08/16/rivington-rallys-cry-meet-with-us-mayor/
The Body http://www.thebody.com/content/81226/neighbors-rally-outside-former-nursing-home-for-hi.html
Articles Pre Vigil:
Lo-Down http://www.thelodownny.com/leslog/tag/rivington-house
Patch https://patch.com/new-york/east-village/calendar/event/20180808/389612/rivington-house-supporters-direct-action-wednesday-august-8th
AM NY https://www.amny.com/real-estate/rivington-house-vigil-1.20342263
And this: an email sent to non-profits and government throughout NY State:
|
FRIDAY, AUGUST 10, 2018
The saga at Rivington House – or, as Gothamist puts it, “one of (New York City) Mayor Bill de Blasio’s biggest black eyes” – continues. At issue is whether the conversion of the former nursing home for HIV/AIDS patients into luxury condos can continue. This planned transformation, approved under de Blasio’s watch, cannot be stopped, he says.
But activists haven’t given up trying to stop developers from taking over the six-story building on Manhattan’s Lower East Side. They attacked with caution tape in protest (Patch has some pretty good photos), hoping that somehow a combination of luck and support from other elected officials and the community can help ensure the building once again serves one of the most vulnerable populations in the city.
– Zach Williams
|
Campaign contributions from Slate Property Group?
(Rivington House buyers and authors of the famous email: Slate Co-Owner: “Do not discuss this deal, the seller [Allure] is very concerned that the city & union [1199] will find out that he is in contract to sell at the price we are buying it which will directly impact his ability to have the deed restriction removed. Once he has it removed, we can do whatever we want.”
Disturbing/surprising News: “For her AG campaign, James took $10,000 from Slate Property Group” [links below]
We are asking that Public Advocate James give Slate $$ back. There should not be even the appearance of buying political influence from those who cost NYS taxpayers this state-of-the-art infectious disease facility and left a low-income community of color without a place for elder or disabled care.
Please, Public Advocate James: return the Slate money.
https://nypost.com/2018/07/28/state-politicians-accepted-illegal-donations-from-corporations/
https://www.cityandstateny.com/articles/politics/campaigns-elections/letitia-james-health-care-group-fundraising.html
http://www.gothamgazette.com/state/7818-inside-attorney-general-candidates-july-campaign-finance-filings
In the United States today “.…this is about who gets to live and who is left to perish today in America” – Mijente